When is All-on-4 the best choice?
Five to 10 years ago, most patients did not know that All-on-4 - fixed jaw implant bridges - existed. Today, patients often ask for this treatment, but are they always in your best interest? Each implant case is different, and it is important that doctors evaluate these five factors BEFORE making a final recommendation for All-on-4 treatment.
5 factors to consider when planning an All On treatment 4
THERE IS NO RULE FOR IMPLANT TREATMENT BUT GUIDLINE. EVERY CASE IS DIFFERENT. The clinician must have a broad understanding of the individual patient's individual factors, thereby making the best treatment plan for that individual. Implantation can often be affected by factors such as tooth misalignment, occlusion, periodontal disease, the size of the space to be restored, and the patient's budget, etc.
It is important that the clinician assesses these factors and listens to the patient's wishes before making a treatment plan. Although these factors must also be considered for the perfect fit patient, for the purposes of this article, I will cover cases only for patients who have lost most of their teeth and who are considering removing them all for the treatment of the All On 4 full-jaw implants.
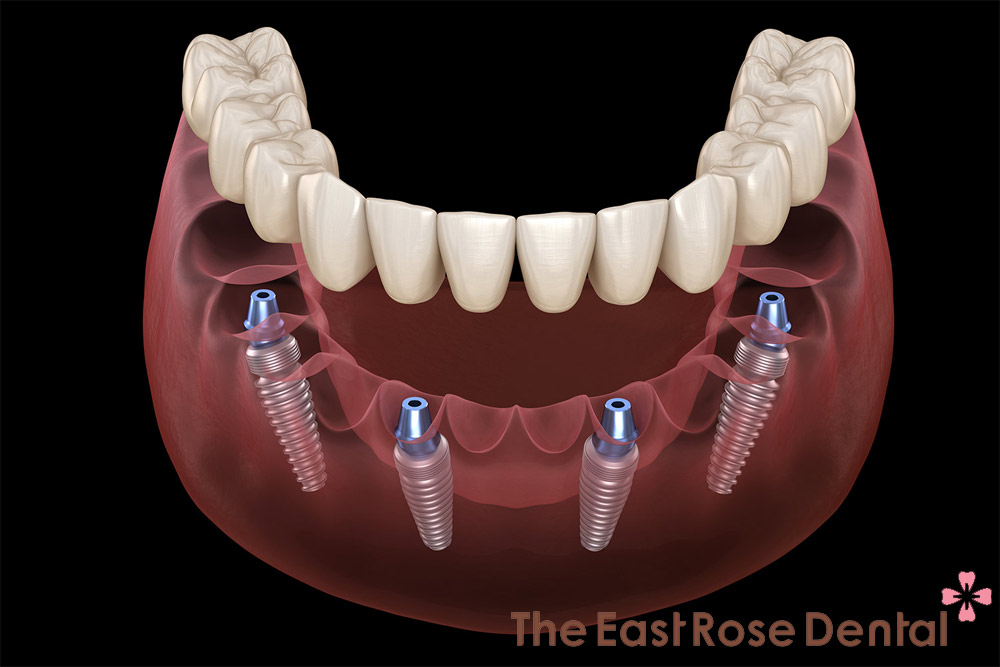
The permanent implant bridge of the entire jaw - commonly known as All-on-4 (figure 1) - is taking over the field of dentistry by storm. These bridges are typically supported by four to six dental implants, made of materials such as acrylic combined with titanium, monolithic zirconia and porcelain on a cobalt-chromium metal frame. This method is often bundled in order to simplify the accountability for each different case. In addition, some facilities promote All-on-4 with their patients that it is the best treatment option for difficult to cure cases.
Will All On 4 always bring the best benefit to the patient? Is All On 4 always great? Under what circumstances will they interfere? This is a very long and complicated topic, but we briefly summarize five factors that The East Rose Dentistry regularly encounter in the course of All on 4 practice:
- Communication, pronunciation and voice problems.
- Difficult to adapt to the bulky thickness of All On 4 bridges.
- Decreased sensation of chewing force
- Bites
- High risk of tooth decay
Let's take a closer look at each of these aspects to see how each may affect the consideration of treatment.
Communication, pronunciation and voice problems
Communication and pronunciation problems are of great concern to the patient. To us, what appears to be a slight flaw in voice could become a major concern for All-on-4 patients? The implant supporting the bridge needs to ensure vertical and horizontal dimensions to bear the force. The vertical dimensions vary depending on the different prosthetic materials, but most bridges require a height of 15 mm or more. Therefore, clinicians are forced to replace more volume of lost teeth to achieve this minimum size. We often have to replace bone mass and soft tissue, even if it's healthy. As a result, the bridge part adjacent to the soft tissue becomes bulkier than the original volume of bone and soft tissue it displaces (Figure 2). Therefore, this can affect pronunciation such as "D," "T" and "N", when the tongue touches the hard palate with the central incisors to produce a sound (figure 3). (1) Likewise, the horizontal volume at the back can affect the "S" sound, where the side contours of the tongue flare up when making a sound. This can lead to lisp. (2)

All on 4 patients need to understand and accept this. They can retrain their tongue from time to time, but this must be a problem for most patients. If language communication is a major concern, clinicians must be prepared to introduce traditional alternative treatments, such as a plan to retain healthy teeth and replace lost teeth with short bridges or individual implant. In case the tooth is badly damaged, it is necessary to remove the entire jaw, which can make the bridge of the entire communication implant, just to replace the missing tooth structure. However, this will often involve more implant, bone graft and expensive prostheses, so the patient will need to prepare for the time and cost of additional treatment.

Difficult to adapt to the thick, bulky pair of All On 4 bridges
In addition to the cumbersome bridge that affects the pronunciation, it can be difficult for the patient to adjust mentally because of the strange feeling brought on by the All-on-4 bridge. They are accustomed to feeling the transition from gum tissue to teeth. With the All-on-4 bridge, the patient senses real soft tissue and then denture gum tissue (the prosthetic gum tissue of the bridge) before switching to the teeth. This can be a big problem for some patients, and sadly they often realize it after the healing process of the surgery. By then, it's too late, we can't do anything to bring them back to their former state of nature again!!!
I recommend having detailed conversations and compromising this before completing a treatment plan so that the patient avoids surprises. I show the patient the All-on-4 model and then the traditional spherical model (they will understand even using the jaw model) (Figures 4 and 5). If the client has huge concern on the inconvenience, then they should consider traditional bridge methods that only replace lost teeth. In order to minimize cumbersome in the prosthesis, both vertically and horizontally, it is more likely that more implants will be needed, more bone grafting to assist in reducing bridge span and avoiding the risk of fracture. The prosthetic intervals may need to be shortened and the implant will be placed backward, which may lead to bone grafting, higher costs and longer treatment time. Patients can choose the All-on-4 bridge after consultation due to its lower cost and reduced treatment time. In any case, when the patient has multiple options to choose from and knows the limitations prior to treatment, they are more likely to accept any compromise.


Decreased sensation of chewing force
This is a major problem that often both doctors and patients ignore, overlook or disregard when recommending All On 4 treatments. Natural teeth have periodontal tissue, present in the periodontal ligament, making teeth sensitive to low forces. This means that you can immediately feel that you are chewing with the lightest chewing force, resulting in high chewing efficiency. The implant abutment has no periodontal ligaments, and requires approximately 10 times more force for the patient to feel like real teeth. Perception after implantation is similar to the case of teeth affected by local anesthesia. This means that it will be difficult for the patient to recognize pre- or excessive occlusal contacts. They can cause excessive bite force due to lack of receptivity. All-on-4 prostheses patients are more likely to bite excessively, have to use much stronger chewing force, but the chewing effect is less effective than real teeth or compared to patients with prostheses but still has some of their own teeth, this can lead to fracture of the All On 4 prosthesis or bone resorption (figure 6).

My All-on-4 patients experience temporary chipping or broken teeth. Always consider the choice of a traditional orthodontic treatment (which can save at least a few teeth) if both jaws are in need of treatment. If this is not possible, consider a staged treatment using your upper jaw before you have real teeth in place for the first few months. You may need to correct your teeth to balance the occlusal plane. Feeling the lower jaw will help the patient avoid the force of the bite too strong and learn to recognize occlusal deviations. After a few months, you can treat your lower jaw. This will give the patient time to develop mechanical receptors in bone tissue - such as muscles, joints and periosteum - to aid in feedback. Upper jaw implants will also benefit from a longer healing time to increase bone integration before being affected by the potentially traumatic force of the bridge on the opposite implant.
Bites
Disruptive habits - such as grinding and chewing irregularly - can affect your treatment decisions. As discussed in the previous section, real teeth can detect force much more easily than implants. Including a few retained real teeth according to your treatment plan can allow the patient to feel the force and bite better (figure 7), which will increase their chances of correcting negative behavior about movement to chew and bite joints

If it is necessary to replace all the teeth you may consider recommending a overdenture with metal bar support (figure 8). Technically, this is still an All-on-4 procedure, but it could change the patient's perception of the fixed bridge. I use the overdenture on metal bar for patients who grind their teeth strongly. The overdenture can be removed at night and replaced with a flat planed anti-grinding tray attached to the bar for retention. This helps to preserve the ultimate prosthesis and reduces the pressure on the implant and supporting bone.

The risk of tooth decay is high
This is a very common situation: For example, a patient visits to The East Rose Dentistry with a condition: The upper jaw has lost all of molars and is currently wearing a full removable denture or the upper jaw All-on-4 - and the lower molars were decayed and some teeth were missing. Patient wants to make All-on-4 lower jaw fixed bridge. The question for me is: Should I preserve the patient's teeth, fill it, restore and preserve all the real teeth, replace the lost teeth with the traditional implant bridge method or will I extract them all for proceeding All On 4 according to patient's request? What are the risks and benefits?
These are my views: If the real teeth are slightly loose and mostly intact, or have cavities, periodontal disease can be saved (perhaps a ceramic crown and a filling, periodontal treatment, root canal ...), I would consider saving them as the risk of developing more periodontal disease or damage from tooth decay may be less than the risk of prosthetic fracture or damage to the complex implant / bone due to excessive chewing or dysfunction if they are removed to make the All On function 4. In this case, I ask the patient to improve their home care, see the dentist more often and significantly reduced sugar intake.
However, this is too much to ask for. The risk of losing these teeth due to tooth decay in the not too distant future may outweigh the risk of a prosthetic fracture or resorption. Perhaps the best treatment for this patient would be to use an overdenture on an All-on-4 metal bar or All On 4 bridge. In addition to the ability to relieve pressure, this treatment will consistent with a simplified oral hygiene procedure. You will want to spend more time with this patient before making a final treatment decision.
Conclusion
We are fortunate to have All On 4 implant technique added to our armory as an ideal option to replace lost teeth.
Here's what I recommend: Offer as many full-fledged prosthesis options as ever, but take time to evaluate the individual options that are best for your patient. Make sure you keep them informed about the obstacles they will need to overcome, not just the benefits of treatment. Take the time to do this and you will have better treatment results and more satisfied patients. Isn't that what we really want?
Services
Working Time
- Monday - Friday: 08:00 - 19:00
- Saturday: 08:00 - 18:00
- Sunday closed
Contact Info
- Hotline 1: (+84) 908 321 455
- Hotline 2: (+84) 931 857 885
- Mobile: (+84) 8 3925 8778
- Phone: (+84)2 838 258 778
- info@dentalrose.net
- rosedentalclinicvn@gmail.com
 English
English  Tiếng Việt
Tiếng Việt

