What is Periodontal Disease and Types of Gum surgery?
How did I get Periodontal Disease?
Periodontal disease begins with bacteria present in the mouth attaching to the teeth. The bacteria collect and multiply, forming a biofilm called dental plaque.
If this plaque is left on the teeth, the adjacent gingival tissues can become inflamed, resulting in the development of gingivitis, an early form of gum disease. Daily flossing and twice-daily brushing with a toothpaste that fights bacteria can help prevent gingivitis.
Plaque and food debris are removed by oral hygiene practices and thus clean the surface of the teeth and eliminate bacterial plaque at the gum line of the teeth. (It needs to be clear from this section that gingivitis is an early form of gum disease that can lead to periodontitis, a serious form of gum disease if left untreated).
However, if plaque and food debris are not removed and oral hygiene practices are not maintained, then gingivitis will get worse and the gum tissue can become more inflamed, bleeding gum can occur, the area between the tooth and gum tissue can become deepened to form a periodontal pocket and periodontal disease can develop.
A periodontal pocket develops as the plaque bacteria from the biofilm continues to accumulate and moves below the gum line. At this point, home care is not very effective in removing dental plaque. If it is left untreated by the dentist or dental hygienist, the biofilm will continue to spread below the gum line and infect the inside of the pocket.
The bacteria in the plaque produce by-products that cause the adjacent soft and hard tissue to degrade, forming a deeper pocket in the process.
This type of advanced periodontal disease can affect the roots of the teeth and they can become infected, too. The teeth may become loose or uncomfortable and the patient will require gum surgery. The patient would be required to have initial therapy to treat diseased periodontal pockets through scaling and root planing.
The dental hygienist would utilize an ultrasonic scaling device to remove plaque, tartar, and food debris below the gum line and would hand scale the tooth and root surface to make it smooth and disease-free. Scaling and root planing can be completed in two to four sessions depending on how much oral disease the patient may have. Thorough oral hygiene procedures would be reviewed with the patient to improve oral care cleaning techniques at home.
Read more: Things to know about dental tartar removal
About Gum Disease Treatment
Non-Surgical Treatments
AAP treatment guidelines stress that periodontal health should be achieved in the least invasive and most cost-effective manner. This is often accomplished through non-surgical periodontal treatment, including scaling and root planing (a careful cleaning of the root surfaces to remove plaque and calculus [tartar] from deep periodontal pockets and to smooth the tooth root to remove bacterial toxins), followed by adjunctive therapy such as local delivery antimicrobials and host modulation, as needed on a case-by-case basis.
Most periodontists would agree that after scaling and root planing, many patients do not require any further active treatment, including surgical therapy. However, the majority of patients will require ongoing maintenance therapy to sustain health. Non-surgical therapy does have its limitations, however, and when it does not achieve periodontal health, surgery may be indicated to restore periodontal anatomy damaged by periodontal diseases and to facilitate oral hygiene practices.
Periodontal Surgery
If you’re diagnosed with gum disease, your periodontist may recommend periodontal surgery. Periodontal surgery is necessary when your periodontist determines that the tissue around your teeth is unhealthy and cannot be repaired with non-surgical treatment.
The Use of Lasers in Periodontal Therapy
Limited research suggests that the use of lasers as an adjunct to scaling and root planing (SRP) may improve the effectiveness of this procedure. In addition, when the lasers are used properly during periodontal therapy there can be less bleeding, swelling, and discomfort to the patient during surgery. However, each laser has different wavelengths and power levels that can be used safely during different periodontal procedures. Damage to periodontal tissues can result if an inappropriate wavelength and/or power level is used during a periodontal procedure.
Gum Graft Surgery
The benefits of gum graft surgery
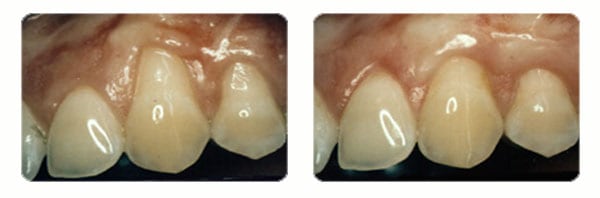
Periodontal procedures are available to stop further dental problems and gum recession and improve the esthetics of your gum line.
- A gum graft can reduce further recession and bone loss.
- It can cover exposed roots to protect them from decay. This may reduce tooth sensitivity and improve the esthetics of your smile.
- Whether you have a gum graft to improve function or esthetics, you often receive the benefits of both: a beautiful new smile and improved periodontal health – your keys to smiling, eating and speaking with comfort and confidence.
Exposed tooth roots are the result of gum recession. Perhaps you wish to enhance your smile by covering one or more of these roots that make your teeth appear too long. Or, maybe you’re not bothered by the appearance of these areas, but the exposed tooth roots are sensitive to hot or cold foods and liquids.
Your gums may have receded for a variety of reasons, including aggressive tooth brushing or periodontal disease. You may not be in control of what caused the recession, but prior to treatment, your periodontist can help you identify the factors contributing to the problem. Once these contributing factors are controlled, gum graft surgery will repair the defect and help to prevent additional recession and bone loss.
Case 1
Case 2

Case 3

Gum grafts can be used to cover roots or develop gum tissue where absent due to excessive gingival recession. During gum graft surgery, your periodontist takes gum tissue from your palate or another donor source to cover the exposed root. This can be done for one tooth or several teeth to even your gum line and reduce sensitivity.
Types of Gum Surgery
1. Gingival Flap Surgery

If pockets are greater than 5 millimeters in-depth, the periodontist would conduct this procedure to reduce the periodontal pockets that were noted in a patient's chart. Most patients who have been diagnosed with moderate to severe periodontitis would go through this procedure.
The periodontist would cut the gum tissue to separate the gum tissue from the teeth, conduct a thorough deep cleaning with an ultrasonic scaling device as well as hand instruments to remove tartar, plaque, and biofilm below the pockets.
2. Gingivectomy

This procedure is conducted to remove excess gum tissue that may be overgrown on the teeth to provide a better area to clean the teeth. The periodontist would numb the patient's gum tissue and cut and eliminate the extra gum tissue in the mouth.
3. Gingivoplasty

This type of gum surgery is used to reshape healthy gum tissue around the teeth to make them look better. If a person has a tooth recession where the gum is pushed away from the tooth, a gingivoplasty can be done.
A gum graft can be done where the tissue is taken from the roof of the mouth (this is called a graft) and then stitched into place on either side of the tooth that is recessed.
After gum surgery, it is important that the periodontist or dental hygienist inform you how to clean the teeth and gum tissue with a toothbrush and antimicrobial fluoride toothpaste, floss, and antibacterial mouth rinse. Please consult your periodontal specialist or dentist for more information on how to care for your gum tissue and teeth after gum surgery.
Mouth-Body Connection

Periodontal disease, a chronic inflammatory disease, is linked to other health risks.
The American Academy of Periodontology seeks to educate the public about research findings that support what dental professionals have long suspected: Infections in the mouth can play havoc elsewhere in the body. For a long time, it was thought that bacteria was the factor that linked periodontal disease to other infections in the body; however, more recent research demonstrates that inflammation may link periodontal disease to other chronic conditions.
Research has shown, and experts agree, that there is an association between periodontal diseases and other chronic inflammatory conditions, such as diabetes, cardiovascular disease, and Alzheimer’s disease. Therefore, treating inflammation may not only help manage periodontal diseases but may also help with the management of other chronic inflammatory conditions.
When an inflammatory condition is suspected or diagnosed, it is important to consult with both a general physician and a dental health professional, such as a periodontist. Sometimes the only way to detect periodontal diseases is through a periodontal evaluation. A periodontal evaluation may be especially important if you:
- Have a high risk of periodontal diseases. Take the AAP risk assessment test.
- Have heart disease, diabetes, respiratory disease, or osteoporosis, or are thinking of becoming pregnant.
- Have a family member with periodontal disease. Research suggests that the bacteria that cause periodontal disease can pass through saliva. This means the common contact of saliva in families puts children and couples at risk for contracting the periodontal disease of another family member.
- Have a sore or irritation in your mouth that does not get better within two weeks.
Services
Working Time
- Monday - Friday: 08:00 - 19:00
- Saturday: 08:00 - 18:00
- Sunday closed
Contact Info
- Hotline 1: (+84) 908 321 455
- Hotline 2: (+84) 931 857 885
- Mobile: (+84) 8 3925 8778
- Phone: (+84)2 838 258 778
- info@dentalrose.net
- rosedentalclinicvn@gmail.com
 English
English  Tiếng Việt
Tiếng Việt

